Weight loss remains the go-to recommendation for most people with type two diabetes. But considering the harm, unsustainability, and limited success of intentional weight loss interventions, isn't it time we asked, "Why are we still focusing on weight"? Rather than prescribing weight loss, more and more health professionals, including myself, are adopting a weight-neutral approach to type two diabetes care to improve HbA1C, blood glucose levels and other biomarkers - while also reducing harm. Keep reading to find out why.
What is weight-neutral diabetes care?
Weight-neutral diabetes care focuses on health rather than weight. It shifts the focus away from weight loss (which we can't control), and encourages self-care behaviours (which we can control), such as eating more fibre, improving our relationship with food, finding joyful movement, reducing stress, and improving sleep and mindfulness.
Rather than promoting dietary restriction and endorsing overexercising to achieve a "goal weight" (which often encourages disordered eating), a weight-neutral or HAES-aligned approach looks at improving biomarkers like HbA1c by increasing nutrition knowledge, improving cooking confidence, recognising non-hunger triggers, promoting body trust, and finding enjoyable ways to move.
Why do health professionals recommend weight loss for people with diabetes?
There's still a strong belief that weight equals health, and that reducing weight will improve health outcomes, especially for people with type two diabetes. However, the reality is while weight loss research shows initial improvements, e.g. improved HbA1C, biomarkers eventually return to starting levels, even if weight loss is maintained. Not to mention, most weight loss studies don't test for harm and are often funded by pharmaceutical and diet companies with a vested interest in recommending weight loss.
Why we don't prescribe weight loss for people with diabetes
Despite what we're taught, we don't have complete control over our weight, and weight loss is more complex than "calories in vs calories out". We can increase our vegetable intake, exercise daily, reduce our alcohol intake, meditate and adopt other health-promoting behaviours, but if we don't reach our "goal weight", we're more likely to give up and return to our old habits.
The harm of weight loss interventions outweighs the benefits, and no weight loss studies show long-term improvements in health outcomes. The results from one of the longest and largest studies on managing type two diabetes using weight loss, the Look AHEAD trial, highlights these limitations. While the dieting group lost 8.5% body weight in the first year and saw improved HbA1c and waist circumference, the strict food intake and exercise regime was unsustainable. Eventually, they started to regain weight, and biomarkers returned to starting levels. Interestingly after 10 years, the results between the dieters and the control group (who received diabetes support and education without a focus on weight loss as an outcome)) were insignificant.
Regardless of the type of diet studied (low-carb diet, intermittent fasting, high protein etc.), they all show promising results in the first 12 months, but few (if any) show long-term health improvements.
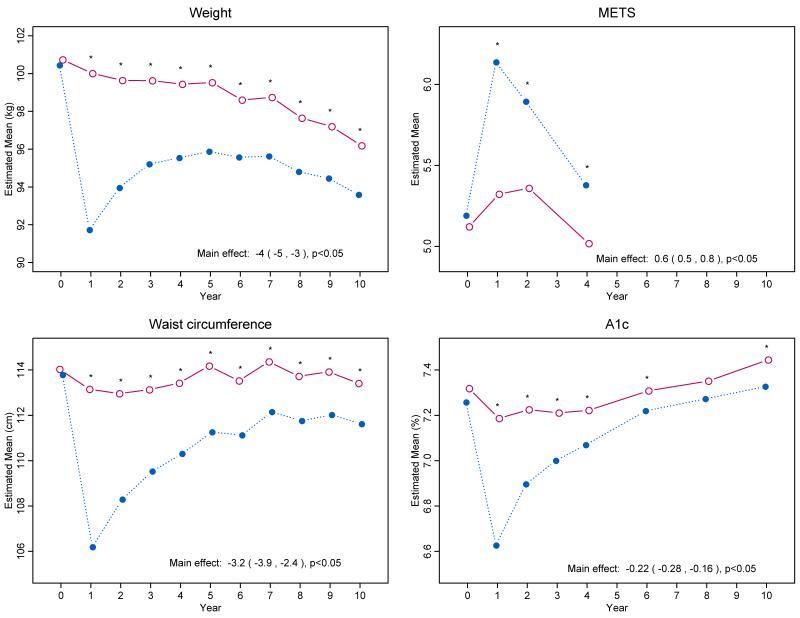
Source: The Look AHEAD research group
Recommending weight loss perpetuates weight stigma
The other reason we don't recommend weight loss is that all people, regardless of body size, deserve compassionate, respectful healthcare that reduces weight stigma. Experiencing weight stigma is detrimental to our health, impacting glucose control, increasing cortisol levels, and the likelihood of experiencing anxiety disorders. Rather than focusing on something we can't control (weight), we empower our clients and give them autonomy by focusing on behaviours they can change and sustain in the long term.
Weight-neutral diabetes care - what we focus on instead
There are forty two factors that can affect blood glucose levels, and weight isn't one of them. That's why instead of recommending weight loss, we focus on the following topics:
Carbohydrate education
Low carbohydrate diets have gained huge attention in the last decade, leading to fear and avoidance of carbohydrates. But carbs are our body's preferred fuel source and essential for keeping us alive and functioning. Telling people to avoid carbohydrates can make people want them more and feel out of control when eating them, potentially leading to poorer glycemic control.
Rather than demonising carbs or labelling them as "good" or "bad", a non-diet approach educates clients about the different types (Low GI vs High GI), timing, quantity and pairing of carbohydrate foods. We discuss the different effects high and low GI foods have on our body, why we aim to eat low GI carbohydrates (e.g. wholegrain bread, wholegrain breakfast cereals, starchy vegetables and legumes) for the most part, and how all carbohydrates can fit within a healthy food intake.
Rather than telling clients what to eat, we provide education and recommend they get curious and think about how foods make them feel. Do you notice you have more energy when you eat low-GI carbs? Do you notice you have less energy when you eat too many high-GI carbohydrates? Do you notice you crave carbohydrate foods when you allow yourself to eat them regularly? Do you feel better if you have smaller meals more frequently throughout the day?
Adding foods, rather than taking away
Rather than creating food fear and anxiety by demonising foods or focusing on the foods to avoid, a non-diet approach shifts the focus towards foods to add. Educating people about the benefits of fibre, protein, unsaturated fats, and low GI carbohydrates in managing blood glucose levels.
Fibre
Fibre can help reduce HbA1c and fasting blood sugar. Eating fibre-rich foods such as whole grains, fruit, vegetables, nuts, and seeds can help slow digestion, allowing glucose to enter the bloodstream more slowly and making it easier for the body to process.
Regular eating patterns
Diet culture encourages us to skip meals and wait prolonged periods before eating. However, this can impact our blood glucose levels. A non-diet goal for someone with type two diabetes might be to eat every 3-4 hours, or helping them self-regulate eating by tuning back into their hunger and fullness signals.
Stress management
The hormonal responses to chronic stress can affect blood glucose levels. That's why we focus on reducing stress, including food stress. Many people with type two diabetes report worrying about eating the "wrong" thing. So when it comes to providing food advice, it's essential to remember there's a fine line between nutrition education and fear-mongering.
Mindfulness
Mindfulness-based approaches can be effective in managing type two diabetes. They address the guilt and shame associated with a diabetes diagnosis, foster self-acceptance and reduce stress. While mindfulness promotes psychological health, it also positively affects physical health, including an improved HbA1C.
Joyful movement
As a result of diet culture, many people have a complicated relationship with exercise. Knowing the physical and mental benefits of movement, we help clients find enjoyable ways to move their bodies, whether walking, yoga, rollerblading, or high-intensity activities.
Harness the power of medication
While lifestyle changes, such as diet and exercise, can help manage type two diabetes, some people will need to also take medication. However, unfortunately, many people hold stigma around taking medication, despite it helping improve insulin sensitivity and reducing the risk of long-term complications. In a non-diet approach, we help people overcome this shame and empower them to use medication as a tool to increase food flexibility.
Let's focus on health, not weight, to improve type 2 diabetes outcomes
Want to learn more about how we can support you in managing your type two diabetes using a weight-neutral approach? Get in touch with our friendly team to book an appointment with one of our non-diet, HAES aligned diabetes dietitians.
References
Armani Kian et al (2018) The Impact of Mindfulness-Based Stress Reduction on Emotional Wellbeing and Glycemic Control of Patients with Type 2 Diabetes Mellitus.
Marisa E Hilliard et al (2016) Stress and A1c Among People with Diabetes Across the Lifespan
Bacon and Aphramor (2011). Weight Science: Evaluating the Evidence for a Paradign Shift.
Carroll et al (2007). Short term effects of a non dieting lifestyle intervention program on weight management, fitness, metabolic risk, and psychological well being in obese premenopausal females with metabolic syndrome.
Flávia M Silva et al (2013) Fiber intake and glycemic control in patients with type 2 diabetes mellitus: a systematic review with meta-analysis of randomized controlled trials

